Raj Sonography & X- Ray Clinic, Baiju Choraha, Nayapura, Guna, Madhya Pradesh, India.
Short Title: Trimester Specific Colour Doppler Study
*Corresponding Author: Lalit K Sharma, MD, Raj Sonography & X- Ray Clinic, Baiju Choraha, Nayapura, Guna, Madhya Pradesh, India E-mail : drlksharma_guna@yahoo.co.in
Keywords: Doppler
Ultrasound, Pre-eclampsia, Fetal Growth Restriction, Delay, Perinatal Care
Established Facts and Novel Insights
Established Facts
- India Has A High Perinatal Mortality Rate.
- There are Several interlinked delays that influence Perinatal outcomes
- Uptake of antenatal care services and ultrasound is suboptimal in India.
Novel Insights
- Integrating Colour Doppler Studies with 1st trimester ultrasound exams can help identify early pregnant women at high risk for preterm preeclampsia and aid in starting prophylactic low dose aspirin for such women
- Integrating Colour Doppler Studies with routine 3rd trimester ultrasound exams can help identify early pregnant women with growth restricted fetuses and aid monitoring of such fetuses
Abstract
Introduction: India has a high perinatal mortality rate that can be attributed in part to the models of delay influencing perinatal care. Integrating Colour Doppler Studies with routine trimester specific ultrasound exams can help reduce delays optimizing perinatal care
Case Presentation : A pregnant woman presenting at 12 weeks of gestation was identified as being at high risk for preterm preeclampsia (PE) and started on low dose aspirin 150mg once daily at bedtime to be continued till 36 weeks or delivery or onset of PE, whichever is earlier. At 32 gestation weeks, she was identified with Stage 1 fetal growth restriction (FGR) based on Doppler studies and advised weekly follow up. At 35 gestation weeks, Doppler studies indicated Stage 3 FGR and early onset fetal acidemia. The woman was referred to a tertiary care center for immediate childbirth and delivered a live baby weighing 1700 gms by a cesarean section.
Discussion/Conclusion. Colour Doppler studies helped optimally initiate low dose aspirin early in the 1st trimester. Colour Doppler studies 3rd trimester helped the early identification of FGR and initiate weekly follow up as opposed to routine follow up after 4 weeks, identify early the progress to stage 3 FGR and fetal acidemia and recommend immediate childbirth. This fetus may not have survived if the routine schedule for ultrasound exam during the 3rd trimester was followed.
India has a high perinatal mortality rate, 36 per 1000 pregnancies, as reported by the National Family Health Survey-4 (NFHS-4) of India .[1] NFHS-4 reported a still birth rate of 0.7% and a neonatal mortality rate of 30 per 1000 live births in India, and a birth weight <2500 grams in 18.2% of live births.[1] Preterm births and low birth weight are the major causes (41.77%) of neonatal deaths in India.[2] The maternal mortality ratio in India was reported as 130 per 100,000 live births in 2014-16 [3]. The NFHS-4 reported that only 58.6% pregnant women had at least one antenatal care visit in the 1st trimester of pregnancy and only 61% of all pregnancies had received at least one ultrasound exam during pregnancy.[1]
Thaddeus and Maine introduced the Three Delays framework, in 1991, to describe obstacles that lead to maternal death [4]. Maternal death can result from the delay: (1) to seek appropriate medical help for an obstetric emergency; (2) to reach an appropriate obstetric facility; and (3) to receive adequate care at the facility. [5,6,7,8,] Pacagnella, et al, critiqued the Three Delays model for its inability to consider underlying factors that contribute to maternal death and lack of consideration for preventative care that reduces maternal mortality [6]. A fourth delay related to community factors [6,9] was recommended as an addition to the 3 delay model.
In this case, we discuss the impact of integrating colour Doppler Studies with routine trimester specific ultrasound exams on the 4 delay model and illustrate how it may help reduce perinatal mortality in India.
Case Report
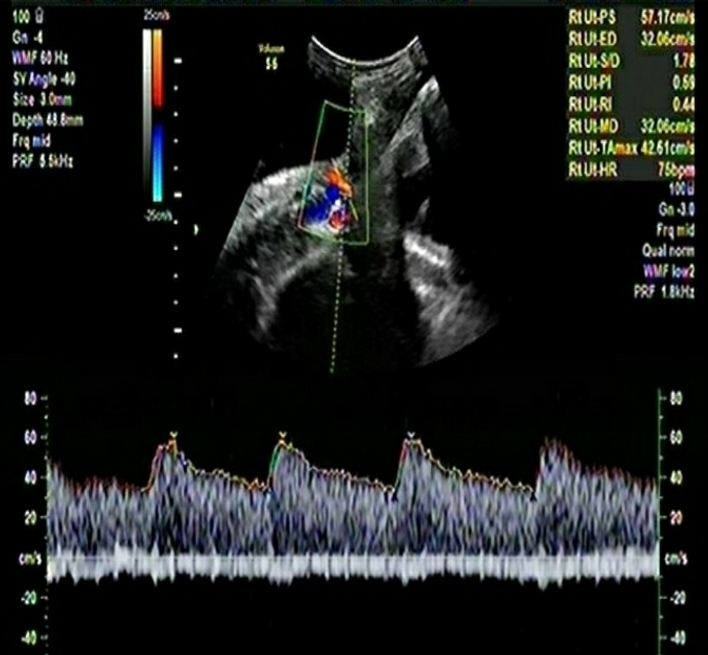
A pregnant woman presented to us at 12 weeks of gestation for routine 1st trimester ultrasound exam. The woman was screened using a combined screening protocol [10] that incorporated clinico-demographic details like age, parity, body mass index, family history of PE, history of PE in previous pregnancies, inter-pregnancy interval, use of assisted reproductive conception, comorbid conditions especially diabetes mellitus, chronic hypertension, systemic lupus erythematosus and anti-phospholipid syndrome. Two readings of the systolic and diastolic blood pressure in both arms were taken simultaneously using validated digital instruments and determination of the mean arterial pressure was done using a standardized protocol. Ultrasound scan for dating of pregnancy and fetal biometry was done through a transabdominal approach, and Colour Doppler study of the right and left uterine arteries and determination of the mean uterine artery PI was carried out. A sagittal section of the uterus was obtained and the cervical canal and internal cervical os were identified. Subsequently, the transducer was gently tilted to the side in the midline and colour flow mapping was used to identify each uterine artery along the side of the cervix and uterus at the level of the internal os. Pulsed‐wave Doppler was used with the sampling gate set at 2 mm to cover the whole vessel and care was taken to ensure that the angle of insonation was less than 30°. When three similar consecutive waveforms were obtained, the Uterine artery PI was measured and the mean Uterine Artery PI of the left and right arteries was calculated. Biochemical markers were not assessed.
The woman was determined to be at high risk for the development preterm PE based on the combined screening protocol algorithm [10] and is used globally to determine risk estimates for preterm PE based on a priori risk factors and based on a 1 in 150 cutoff. The risk calculator is available free of charge at https://fetalmedicine.org/research/assess/preeclampsia. Consistent with current evidence based recommendations for the management of pregnant women at high risk for preterm PE, the woman was advised low dose aspirin at 150mg once daily at bedtime to be continued till 36 gestation weeks.
The pregnant woman was initially reluctant to start low dose aspirin but started the schedule after repeated counselling in alignment with the managing obstetrician. She was advised follow up Doppler and ultrasound exams at 22, 26 and 30 weeks of gestation but did not come for the follow up exams. After repeated telephonic contact and counselling over the telephone, she came for the repeat ultrasound exam at 32 weeks.
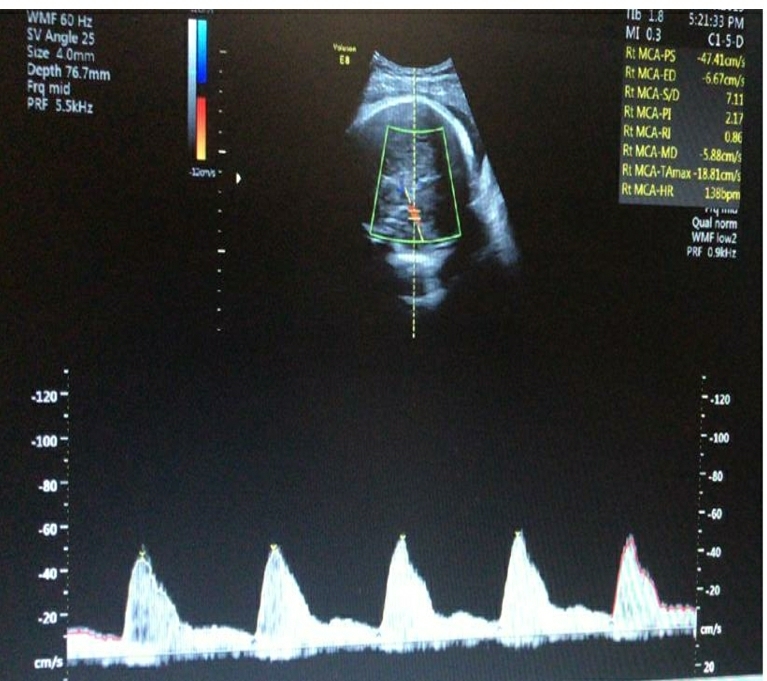
Doppler and ultrasound exams at 32 weeks showed a live fetus with Stage 1 FGR. The estimated fetal weight (EFW) was 1 centile and Abdominal circumference was 11th centile. Umbilical Artery Doppler PI was 96th centile, the middle cerebral artery Doppler PI was 1 centile and the Cerebro-Placental ratio was 1 centile. She was advised weekly follow up for repeat exams and monitoring of the health of the fetus. The pregnant woman and her family were reluctant for weekly exams but provided consent after counselling. The status of the fetus remained unchanged till 34 weeks of gestation.
At 35 weeks of gestation, Doppler study showed absent end diastolic velocity in the umbilical artery and EFW 0 centile with normal liquor. The Ductus Venosus was explored and the PI was 99th centile. The clinico-demographic and Doppler parameters were assessed using the Barcelona algorithm available online and the fetus was determine to have progressed to Stage 3 FGR with early acidemia.
She was advised administration of antenatal corticosteroids for fetal maturity and referral to a tertiary care center for immediate delivery. The family were reluctant to plan for immediate childbirth but agreed after repeated counselling and explanation of the Doppler study findings.
Communication was established with the managing obstetrician at the tertiary care center and details of the Doppler and ultrasound exams were shared. A caesarean section was done for immediate childbirth and a live baby weighing 1700 grams was delivered. The child was live and healthy a week after delivery.
Discussion
This case highlights the importance of using a combined screening protocol to estimate the risk for preterm preeclampsia and fetal growth restriction in the 1st trimester integrating colour Doppler studies with routine ultrasound exam. In the 3rd trimester, the integration of colour Doppler studies aids in the early identification and monitoring of the progress of FGR guiding decision making pertaining to childbirth. This case highlights the impact the screening, staging, and monitoring protocols and the potential impact of the 4 delay model on perinatal mortality rates.
The three delay model of Thaddeus and Maine [4] identified the three delays as a) delay to seek care, b) delay to reach help and c) delay to receive adequate help. The fourth delay [6,9] was added later and identified as related to community factors. The four delays, in isolation or in combination, contribute significantly to maternal death and are usually interlinked. Previous studies have reported that most maternal deaths occur due to the 1st delay (seeking care), however, the third delay (to receive adequate help) is the most significant.[11] Studies have also emphasized the need to consider multiparous women, women with little or no education and accessibility of services for the poor and the “distance-decay” phenomenon in reaching services.[8] Studies have shown that pregnant women in vulnerable settings often lacked a certain awareness of their healthcare needs and relied on their partner’s/husband’s and/or mother’s advice regarding seeking care. [12] The four delay model is built on a framework is underpinned by Social Constructivism and overlaps with theories of empowerment, participatory communication, social change, socio-ecology and public health.
The first to fourth delays are influenced by the socioecological determinants including knowledge, age, economic status, and social support. [9] The resources of the family and the community and its engagement and willingness to allocate or reallocate resources can also impact the delays. [9] These also include the availability of human and natural resources, transport facilities and good roads within the community and the infrastructure to access them. Family and Community resourcefulness also plays a role in the socioecological determinants of maternal health.
The integration of a combined screening protocol incorporating colour Doppler Studies with routine trimester specific ultrasound exams can help early identification of problems and partly address the first delay of seeking care as well as the 3rd delay of receiving adequate and appropriate help. In this case, we want to highlight the importance of the fourth delay. In this case, we had to repeatedly counsel the woman and her family to start prophylactic low dose aspirin and to return for follow up exams. Despite repeated counselling on the need for follow up exams, the woman missed the entire 2nd trimester of screening. Several rounds of counselling were required for the woman to return for the 3rd trimester exam and to continue screening protocols once she was identified with Stage 1 FGR. Part of the reluctance to continue with the screening protocols was its relative “newness”; other members of the family did not recollect being followed up in this manner. Additionally, the woman looked healthy externally and hence there was a reluctance to believe something may affect the fetus and a doubt whether commercial considerations were overriding the recommendations for follow up exams. Once stage 3 FGR was identified, the woman had to be referred to a tertiary care facility approximately 180 kms away, necessitating the family to allocate resources for transport and stay. Fortunately, the family was convinced and made the effort to reach the tertiary care center. We discussed the case with the obstetrician at the tertiary care center emphasizing on the Doppler findings suggestive of early acidemia setting in and a decision for immediate childbirth by a cesarean section after clinical examination was made.
The routine schedule for 3rd trimester ultrasound at 32 weeks, when fetal biometry and growth is normal, is to recommend a follow up screening after 4 weeks. In this case, the fetus biometrics were normal but Doppler identified the early onset of FGR. This allowed the initiation of a weekly follow up protocol that helped early identification of the progress to stage 3 FGR. [13] The baby was delivered before the 36th week when the routine follow up may have been scheduled if recommendations were based without integrating colour Doppler findings. It is possible that this fetus may not have survived till then or may have developed neonatal consequences from acidemia.
This case highlights that integrating colour Doppler Studies with routine trimester specific ultrasound exams as part of a combined screening protocol can positively influence the delays influencing perinatal outcomes. Repeated counselling and communication with the pregnant woman, her family and other stakeholders in her health care is essential to ensure optimal care.
References
- International Institute for Population Sciences (IIPS) and ICF. 2017. National Family Health Survey (NFHS-4) 2015-16: India. Mumbai: IIPS
- Million Death Study Collaborators, Bassani DG, Kumar R, et al. Causes of neonatal and child mortality in India: a nationally representative mortality survey. Lancet. 2010; 376:1853–1860.
- Niti Ayog, India. Maternal Mortality Ratio (per 100,000 live births). Accessed online from https://www.niti.gov.in/content/maternal-mortality-ratio-mmr-100000-live-births on Sep 2, 2019
- Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994; https://doi.org/10.1016/0277-9536(94)90226-7
- Barnes-Josiah D, Myntti C, Augustin A. The “three delays” as a framework for examining maternal mortality in Haiti. Soc Sci Med. 1998; https://doi.org/10.1016/S0277-9536(97)10018-1.
- Pacagnella RC, Cecatti JG, Osis MJ, Souza JP. The role of delays in severe maternal morbidity and mortality: expanding the conceptual framework. Repro Health Matters. 2012; https://doi.org/10.1016/S0968-8080(12)39601-8.
- Saving Lives at Birth https://www.savinglivesatbirth.net/blog/12/02/01/meet-innovator-moi-university-school-medicine.
- White K, Small M, Frederic R, Joseph G, Bateau R, Kershaw T. Health seeking behavior among pregnant women in rural Haiti. Health Care Women Int. 2006;27(9):822–38.
- MacDonald, T., Jackson, S., Charles, M. et al. The fourth delay and community-driven solutions to reduce maternal mortality in rural Haiti: a community-based action research study. BMC Pregnancy Childbirth 18, 254 (2018) doi:10.1186/s12884-018-1881-3
- Rolnik DL, Wright D, Poon LCY, et al. ASPRE trial: Performance of screening for preterm pre‐eclampsia. Ultrasound Obstet Gynecol. 2017; 50: 492– 495.
- Barnes-Josiah D, Myntti C, Augustin A. The “three delays” as a framework for examining maternal mortality in Haiti. Soc Sci Med. 1998; https://doi.org/10.1016/S0277-9536(97)10018-1.
- Babalola SO. Factors associated with use of maternal health services in Haiti: a multilevel analysis. In: Rev Panam Salud Publica; 2014. https://www.scielosp.org/scielo.php?pid=S1020-49892014000600001&script=sci_abstract&tlng=es.
- Figueras F, Gratacós E. Update on the diagnosis and classification of fetal growth restriction and proposal of a stage-based management protocol. Fetal Diagn Ther. 2014;36(2):86-98. doi: 10.1159/000357592.