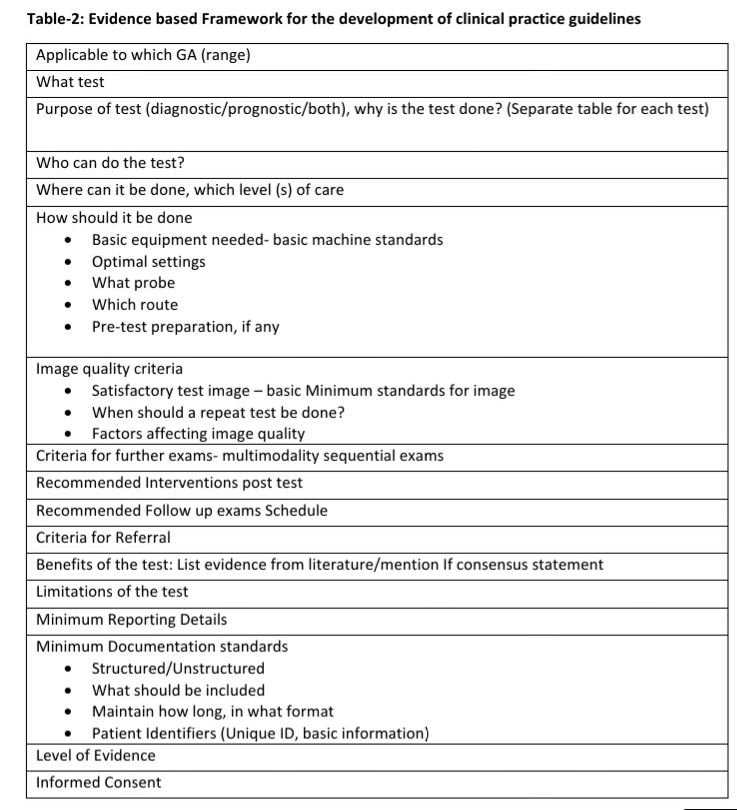
The Utility of mean Uterine artery pulsatility index in prediction of pre-eclampsia -A position paper.
Author: Dr Nivedita Biradar, KREST Fellow in Fetal Radiology and Fetal Medicine, Delta Scans, Bengaluru Pre-eclampsia and other hypertensive disorders…